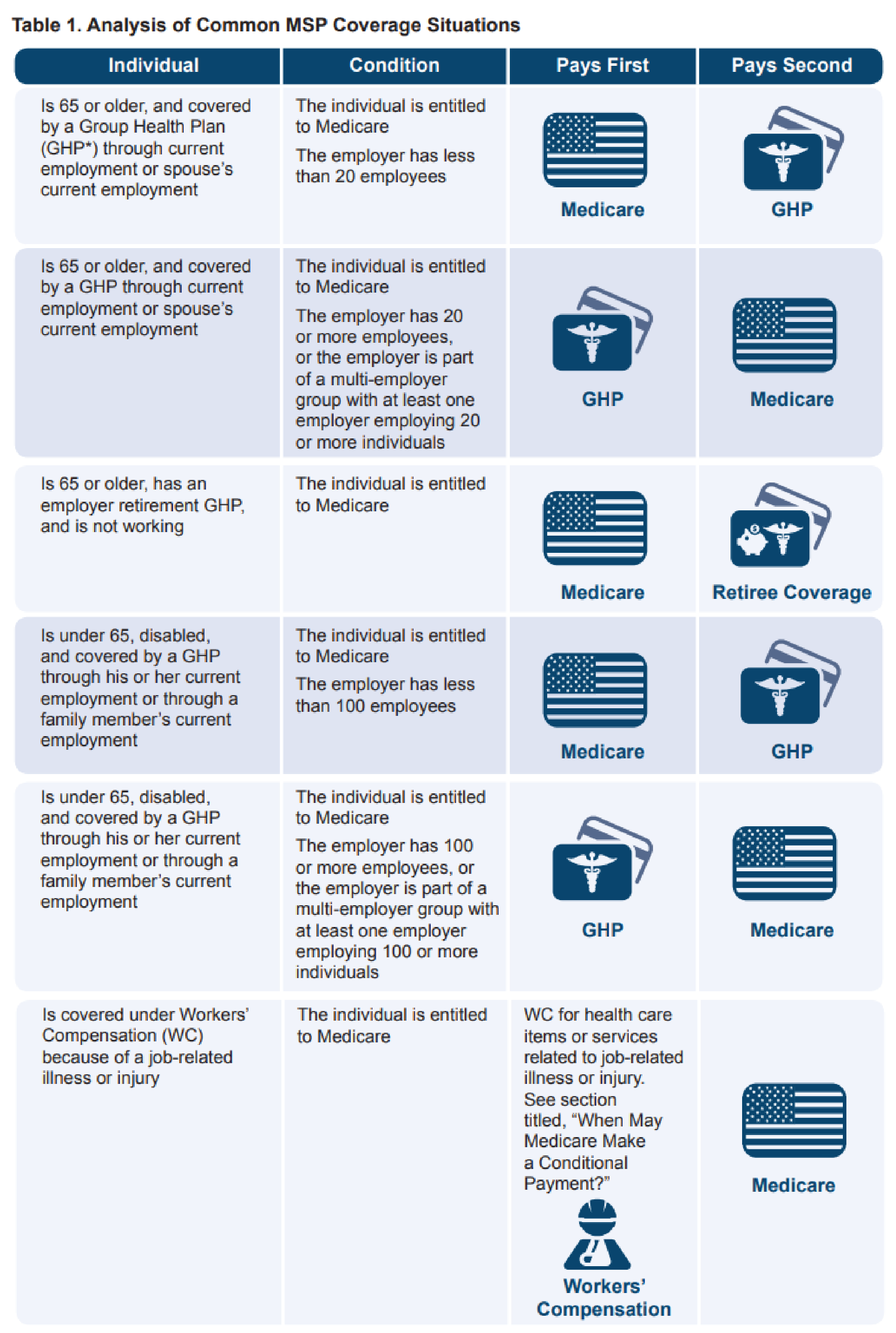
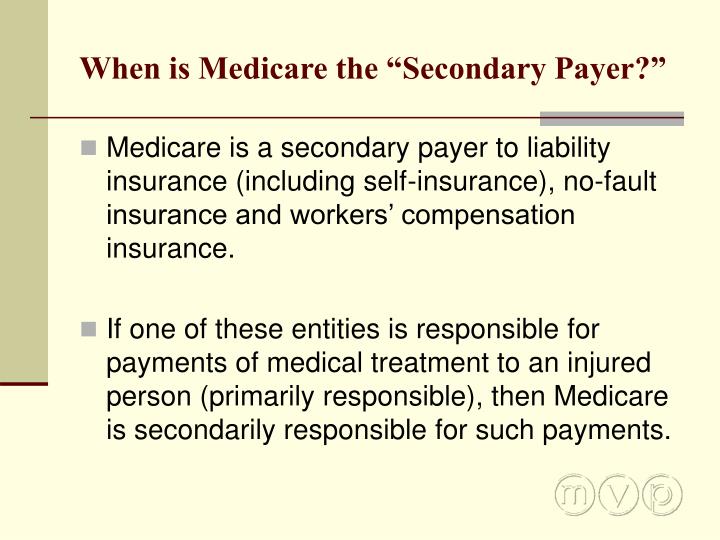
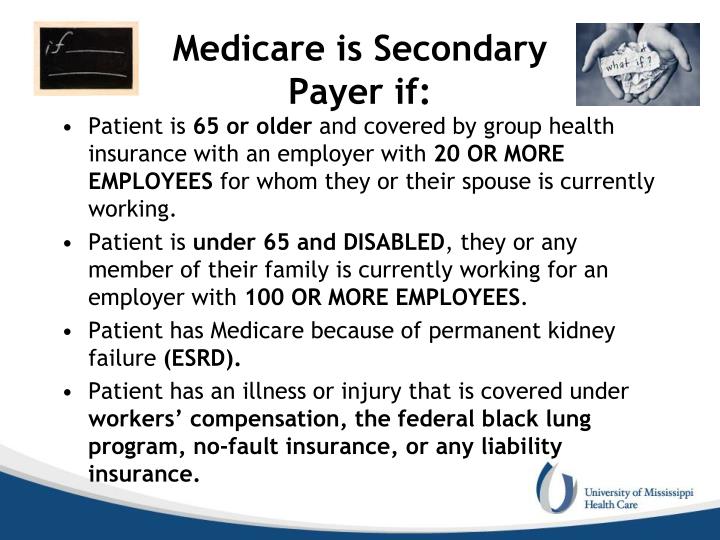
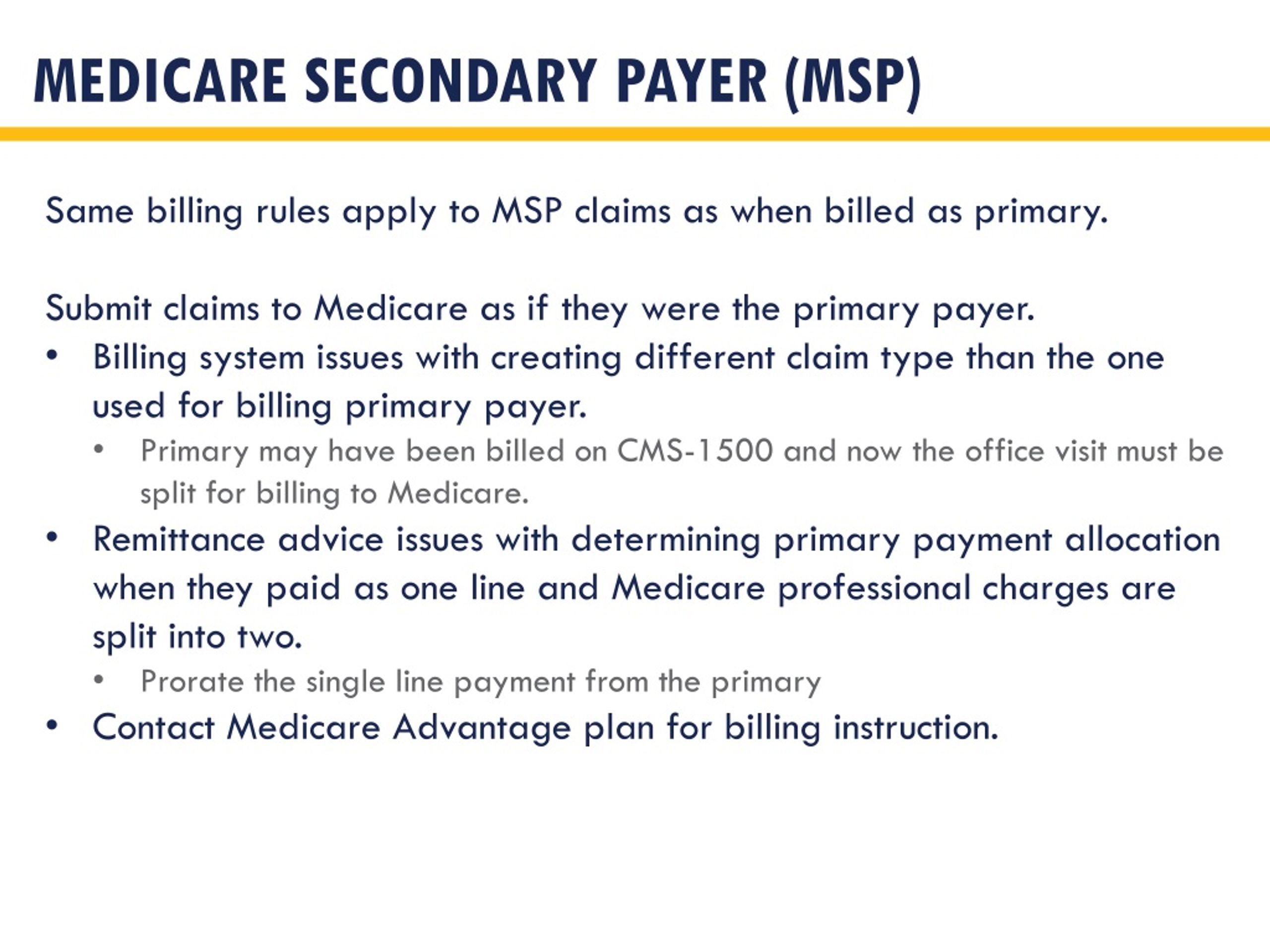
Medicare Secondary Payer Fact Sheet - What is msp and what are the msp provisions? The medicare secondary payer (msp) rules are complex and. How do i identify payers primary to medicare? When must msp records be updated. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. What are a provider’s msp responsibilities?
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. What is msp and what are the msp provisions? Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. When must msp records be updated. The medicare secondary payer (msp) rules are complex and. What are a provider’s msp responsibilities? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. How do i identify payers primary to medicare?
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. How do i identify payers primary to medicare? The medicare secondary payer (msp) rules are complex and. When must msp records be updated. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. What are a provider’s msp responsibilities? What is msp and what are the msp provisions? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or.
PPT Chapter 12 Commercial Insurance PowerPoint Presentation, free
How do i identify payers primary to medicare? Any entity providing items and services to medicare patients must determine if medicare is the primary payer. The medicare secondary payer (msp) rules are complex and. What are a provider’s msp responsibilities? When must msp records be updated.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. The medicare secondary payer (msp) rules are complex and. What are a provider’s msp responsibilities? Pursuant to 42 cfr § 411.100, and.
What is Medicare Secondary Payer? Ametros
What is msp and what are the msp provisions? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals.
PPT RHC BILLING 101 PowerPoint Presentation, free download ID1595196
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance. The medicare secondary payer (msp) rules are complex and. What is msp and what are the msp provisions? When must msp records.
PPT MSP Presentation Background & Basics Presented by Keith Ewing
What is msp and what are the msp provisions? What are a provider’s msp responsibilities? The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. Any entity providing items and services to medicare patients must determine if medicare is the primary payer..
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
The medicare secondary payer (msp) rules are complex and. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. What is msp and what are the msp provisions? How do i identify payers primary to medicare? What are a provider’s msp responsibilities?
Understanding Medicare Secondary Payer (MSP)
Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. What are a provider’s msp responsibilities? The medicare secondary payer (msp) rules are complex and. When must msp records.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare. When must msp records be updated. What are a provider’s msp responsibilities? What is msp and what are the msp provisions? How do i identify payers primary to medicare?
PPT CHAA Examination Preparation PowerPoint Presentation ID4372885
How do i identify payers primary to medicare? When must msp records be updated. Any entity providing items and services to medicare patients must determine if medicare is the primary payer. The medicare secondary payer (msp) rules are complex and. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your.
PPT Provider based billing PowerPoint Presentation, free download
How do i identify payers primary to medicare? What is msp and what are the msp provisions? Any entity providing items and services to medicare patients must determine if medicare is the primary payer. Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or.
Any Entity Providing Items And Services To Medicare Patients Must Determine If Medicare Is The Primary Payer.
The medicare secondary payer (msp) rules are complex and. What are a provider’s msp responsibilities? When must msp records be updated. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your health care is paid for and what you can expect from the way medicare coordinates with other insurance.
How Do I Identify Payers Primary To Medicare?
Pursuant to 42 cfr § 411.100, and further specified in § 411.170 and § 411.172, medicare pays secondary to ghp coverage for individuals age 65 or over if the ghp coverage is by virtue of the individual's current employment status or. What is msp and what are the msp provisions? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. The centers for medicare & medicaid (cms) has rules for determining when other types of insurance such as an employer’s group health plan must pay primary to medicare.